Immuno 101
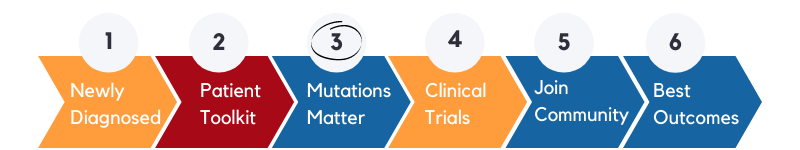
Mutations Matter
Peer to peer – Patient to patient
Sharing knowledge, experience, and wisdom from experienced patients and caregivers to newly diagnosed patients and their community of supporters is essential. The content of this page contains a starting point.
Remember everyone begins from a zero-knowledge point, so find a quiet relaxing place to watch these videos at your own (unhurried) pace. Do not worry about all the foreign items and jargon, just follow the storyline in the first instance, you will find that most of the important bits will sink in over time.
As a cancer challenge moves forward and results begin to arrive from testing, more specific discussions regarding treatment options will be discussed. The content of this page will give you a better understanding, which will increase your confidence and participation or support.
Successful patients share common traits and decisions.
It begins with an open mind and a basic discipline to learn and apply.
Note: Molecular Profiling of a biopsy (by a Laboratory) is described in many different ways –
- Genomic Testing
- Genomic Sequencing
- Biomarker Testing
- Tumour Testing
Terminologies and words
Unfortunately, there are many terms, words, and descriptions within the medical profession to describe the exact same thing. This is confusing initially. The beginning example is “Bile Duct Cancer” is Cholangiocarcinoma. Also Klatskin and hilar (perihilar) are the same, Klatskin being the outdated description. As you will have observed above molecular & genomic profiling or sequencing are essentially the same thing.
Our Primary Focus
The Cancer Toolkits’ primary focus is to EDUCATE – EQUIP – EMPOWER the patient and their whole community of supporters to ensure that the most current and on-point information is delivered.
Dr. E. John Wherry discusses the basics of the immune system, immunotherapy, and cancer.
Immunotherapy continues to transform cancer treatment across several cancer types and shows incredible promise for the future of all cancer care. But what is immunotherapy and how does it work? How is immunotherapy different from other types of cancer treatment?
Dr. E. John Wherry explains how our immune system works, breaks down the complex science underlying immunotherapy into basic concepts, describes the different types of immunotherapy, and discusses potential side effects and benefits that patients can anticipate.
Biomarkers are known indicators.
Cancer biomarkers are biological molecules produced by the body or tumor in a person with cancer. Biomarker testing helps characterize alterations in the tumor. Biomarkers can be DNA, RNA, protein, or metabolomic profiles that are specific to a tumor. Knowing a biopsy’s biomarker results is essential knowledge for therapeutic decision-making, and for treatments such as immunotherapy.
This video is a good starting point
This video shows how the checkpoint pathway works and what happens when an immunotherapy treatment introduces checkpoint inhibitors.
Below is a grassroots interpretation of what this video is wanting you to learn
A Checkpoint Pathway is created when an activated killer T-Cell double-checks with the target cell it is about to destroy. It does this to ensure that is not making a mistake and destroying a healthy cell.
T-Cells have a ligand protruding out from their surface – they are called PD-1 ligands.
Healthy cells express the corresponding ligand from their surface when a killer T-Cell approaches. This corresponding ligand is called a PD-L1 ligand.
Think of a friendly handshake when PD-1 meets a PD-L1. This handshake deactivates the attack and the T-Cell moves away.
Cancerous mutated cells have learned to use this handshake to their advantage and express PD-L1 on their surface when an activated T-Cell approaches, thus shaking hands like old mates and avoiding being destroyed.
Checkpoint Inhibitors introduced by immunotherapy treatments interfere with this handshake by blocking the PD-1 ligand on the surface of an activated killer T-Cell. This blocking prevents the handshake, and the already activated killer T-Cell had no other reason but attack and destroy the cell it was targeting.
So now you can see the importance of discovering PD-L1 in a biopsy (tissue sample) early on. The presence of PD-L1 technically means the patient has a powerful treatment option or can be included in a clinical trial
Note about the presence of PD-L1
Most often PD-L1 is found in an IHC test of the biopsy. If PD-L1 is discovered on this test, it potentially indicates how the cancer is hiding from the immune system, it also indicates that an immune checkpoint inhibitor (immunotherapy) could be successful.
Dr. Charles Drake (16 mins)
Dr. Drake provides an introduction to the basics of immunotherapy, using the immune system to fight cancer. He also covers checkpoint inhibitor therapy (ie PD-1), CAR T cell therapy, oncolytic virus therapy, and therapeutic cancer vaccines.
PD-L1/PD-1 Pathway: (2:43 mins)
How does immunotherapy fight cancer? If you take the brakes off the immune system, you can unleash an attack on cancer cells. PD-1/PD-L1, is a vitally important immunotherapy discovery illustrated in this video.
AstraZeneca (1 min)
The role of PD-L1 Expression and how immunotherapies may target PD-L1 in patients with bladder cancer.
As you move through this video and content, the term MMR and dMMR will emerge.
MSi-high is a downstream result of a faulty MMR system, but more on that later.
Microsatellites are parcels that contain strings of DNA code, these parcels are replicated continuously. Microsatellite Instability occurs when the strings of DNA contained within the microsatellites, begin replicating incorrectly creating errors in our DNA code. Note: Errors are normal
In summary, the level of MSI ie MSi-High, or low is a direct result of our body’s MMR Spellchecker failure. See next section dMMR
MMR is our body’s DNA Spellchecker.
- MMR – Mismatch Repair is our body’s repair genes that repair all our DNA replication errors.
- dMMR – Deficient Mismatch Repair is a term used to describe a failure in the MMR Repair system.
MMR is made up of 4 primary genes.
MLH1, MSH2, MSH6, and PMS2
Deficient Mismatch Repair happens when one or more of the 4 MMR proteins is absent and as a result, the MMR is not functioning correctly and DNA replication mistakes continue unchecked. These mistakes lead to microsatellite instability and cell mutations.
A little confusing
When watching the video below focus mainly on the IHC test explanation. IHC is the test that is carried out on the biopsy sample and picks up if it contains Msi-high.
This is the total number of mutations (changes) found in the DNA of cancer cells. Knowing the tumor mutational burden may help plan the best treatment.
Recently, a high tumor mutational burden (TMB) has been identified as a genetic signature that is associated with a favourable outcome for immune checkpoint inhibitor therapy.
Note about the presence of CTLA-4
Most often CTLA-4 is found in an IHC test of the biopsy. If CTLA-4 is discovered on this test, it potentially indicates how the cancer is hiding from the immune system, it also indicates that an immune checkpoint inhibitor (immunotherapy) could be successful.
As with PD-1, CTLA-4 is also a checkpoint ligand expressed on the surface of a T-Cell. To help simplify their roles (very simplified)…
- The role of CTLA-4 is to prevent the initial activation of a T-Cell
- The role of PD-1 is to deactivate an already activated T-Cell
- Immune Checkpoint Inhibitors (Immunotherapy) interfere and block these two Checkpoints from being able to engage, thus allowing the T-Cell to continue on and attack the cancerous cell.
Ask good questions
We have assembled a list to give you a head start – this list is for bile duct cancer patients but is essentially the same across all solid cancer groups.
Terms used in the order of appearance
Note: The medical community language and description are not always in sync. Different names and terms are used. This is confusing to the patient and caregiver, we try our best to overcome this.
Caregiver
The person who helps you function on an everyday basis
Advocate
People who can speak up, advance the patient and caregiver questions, and generally support the effort. Often patients and their Caregivers have several advocates who have different skills
Clinical Trial
Clinical trials are a type of research that studies new tests and treatments and evaluates their effects on human health outcomes.
Tumor
Tumors are a mass of tissue that’s formed by an accumulation of abnormal cells. Normally, the cells in your body age, die, and are replaced by new cells. With cancer and other tumors, something disrupts this cycle.
Primary Tumor
This is the original tumor location
Biopsy
This is a tissue sample that is obtained from the actual tumor.
Immunohistochemical – IHC
A test that stains the biopsy sample with a chemical solution to highlight the presence of known biomarkers.
Biomarkers
A biological molecule found in blood, other body fluids, or tissues that is a sign of a normal or abnormal process, or of a condition or disease. A biomarker may be used to see how well the body responds to a treatment for a disease or condition.
Immune Checkpoint
The Immune Systems killer T Cell has a failsafe switch to turn off any accidental attack on a healthy cell. Cancer has learned how to turn off this switch and continue growing.
Immune Checkpoint pathway
The Immune Checkpoint pathway refers to the interaction between the killer T Cells and the surface of a normal cell. The T Cell has a PD-1 ligand on its surface and a healthy cell has a PD-L1 ligand on its surface (a matching pair), when these two meet and interact it turns off the unwanted T Cell attack – Cancer has learned to hide behind this by expressing PD-L1 when a T Cell approaches.
Immune Checkpoint Inhibitor -ICI
This is an immunotherapy drug – a monoclonal antibody designed in a laboratory that interferes with the T Cell’s “Checkpoint Switch” by locking in the “On” position, so the T Cell can continue and illuminate the cancerous tumor.
Keytruda
Keytruda is a monoclonal antibody created in a laboratory and infused into the patient. Keytruda is not a chemotherapy treatment.
Monoclonal Antibodies
Monoclonal – means they are designed to perform a single purpose or task.
- Monoclonal antibodies are made in a laboratory and are used to block the activity of abnormal proteins detected on infected cells. They are often designed to attach themselves to protein receptors on the surface of cells infected by viruses, essentially acting as a broadcasting beacon /marker that alerts our immune system to attack.
- Monoclonal antibodies have also been developed to be used as an immunotherapy and help turn the immune system against a cancerous cell. For example, some monoclonal antibodies mark cancer cells so that the immune system will better recognize and destroy them, while others such as Keytruda act as a blocking mechanism. See the video section.
Immunotherapy
Think of immunotherapy drugs as specially designed actions that interfere with what is driving the tumor growth. A lot like a computer has code that goes wrong and a new “patch’ or string of code has to be added as a workaround. Immunotherapy is being referred to as the first ever cancer cure – a modern-day penicillin moment in history.
Monoclonal
Simply this is an antibody designed in the laboratory to perform one single function/purpose.
Molecular Profile
This is a comprehensive examination of a biopsy sample. It examines the genetic and genomic makeup of the sample provided.
Genetic
Genetics is a term that refers to the study of genes and their roles in inheritance – in other words, the way that certain traits or conditions are passed down from one generation to another. Genetics involves scientific studies of genes and their effects. Genes (units of heredity) carry the instructions for making proteins, which direct the activities of cells and functions of the body. Examples of genetic or inherited disorders include cystic fibrosis
Genomic
Genomics is a more recent term that describes the study of all of a person’s genes (the genome), including interactions of those genes with each other and with the person’s environment. Genomics includes the scientific study of complex diseases such as cancer because these diseases are typically caused more by a combination of genetic and environmental factors than by individual genes. Genomics is offering new possibilities for therapies and treatments for some complex diseases, as well as new diagnostic methods.
What is the difference between Genetic & Genomics testing
Molecular Profiling
IHC Test & NGS (Genomic Profiling )
Notes: NGS = Next Generation Sequencing – a more modern name for genomic testing. Refers to MSi testing, IHC Test (2mins), PD-L1 and TMB – Tumor Mutational Burden
Molecular Profiling
Checkpoint Pathway Explained
Immunotherapy 101 explained
Refers to MSI, TMB,
How Keytruda works
Keytruda, combinations and side effects
Cancer explained
Catergories of Cancer
NCI Directory of Medical Terms
APC
Antigen Presenting Cells: The immunes messengers.
B Cells
B Cells have 2 primary functions (1) Produce the ‘antibodies’ and (2) Produce memory cells for any future threats.
CTLA-4
A Check Point protein that sits on the surface of the T Cells. They prevent mistake attacks on healthy cells.
Car T Cells
A new innovating immunotherapy technique
IHC
Immunohistochemistry test chemically stain the tissue biopsy looking for a response that indicates the presence of PD-L1, MSi, HER2 that are known match’s for current Immunotherapy treatments.
Ligand
An elongated strand of protein receptor that anchors to a cell surface. (ie PD-L1 is a Ligand receptor)
Molecular Profiling
Provides a DNA road map of the tumors fingerprint (Genomic) and your hereditary fingerprint (Genetic)
Microsatellites
Microsatellites are stretches of DNA that contain a repetitive sequence of nucleotides
Nucleotides
Nucleotides are the repetitive strings of DNA code that make us – us. example of a code string; “AAAAA or CGCGCGCG” (codes are short tandem sequences that replicate)
MSI
Is a measure of Microsatellite Instability
MSI-LOW
Is a low recorded measure of Microsatellite Instability.
MSI-HIGH
Is a high recorded measure of Microsatellite Instability.
MSS
Is Microsatellite Stable, which means no instability is present
MMR
Mismatch Repair is the DNA repair pathway that plays a key role in maintaining our genomic stability. MMR is our “Spell Checker” correcting any errors in our DNA replication process as they occur.
MMR
Is made up of 4 proteins (MLH1, MSH2, MSH6, & PMS2 )
Think of MMR as our bodies DNA Spell Checker – DNA replication often goes wrong and the MMR genes correct this.
dMMR
Deficient Mismatch Repair means that one or more of the 4 MMR proteins absent and as a result, the MMR is not functioning correctly and is described as deficient
Think of dMMR as our bodies DNA Spell Checker that has become broken and as such is letting DNA replication mistakes continue unchecked.
TMB
Means Tumour Mutation Burden
High TMB is gathering attention as a biomarker indicator that immunotherapy treatments could prove successful.
PD-L1
means Programmed Death Ligand 1 – a cluster protein that generally coats and protects healthy cells from the immune systems T Cells
PD1
Is an Immune Check Point Inhibitor – its function is to switch off a T Cell attack. It does by binding and communicating with the PD-L1 anchored to a cell surface.
PD-1/ PD-L1 Pathway
A communication pathway/channel that dampens or deactivates (switches off) an immune response – (T Cell attack) on healthy cells.
HER2
Is a growth receptor gene often found on the surface of breast cancers cells – too many receptors cause cells to grow and divide too quickly, Immunotherapy treatments have shown positive results in blocking this growth pathway.
Empowering the “Newly Diagnosed Patients” with today’s breakthrough information today!
The Globally Connected Patient has become a critical tipping point in realizing the cancer cure, transcending traditional boundaries and red-tape, as we share our results directly to each other. A peer to peer patient and caregiver collective, the informational sum of Cancer Experiences, Knowledge, Wisdom’s, and results connected in realtime. This is something that the international medical community cannot do.
A modern phenomenon unfolding via the power of targeted social media, unclogging, and delivering “TODAY’S breakthrough results TODAY! – Highly Targeted knowledge delivered into the hands of those most in need -“The Newly Diagnosed Patient and Caregiver”
We sincerely hope that the information on this page leads you and your family back to solid ground and happier outcomes,
Yours Sincerely
Steve and Claire Holmes
www.steveholmes.net.au
What are PD-1 and PD-L1 biomarkers
CANCER CELLS MAY USE THE PD-1 PATHWAY TO HIDE FROM T CELLS
Important View Immuno 101
The immune system is your body’s natural defense against disease. The immune system sends certain types of cells called T cells throughout your body to detect and fight infections and diseases—including cancer.
Cancer cells may use the PD-1 pathway to hide from T cells. This stops T cells from attacking cancer cells and allowing cancer cells to grow and spread.
PD‑1 = programmed death receptor-1
PD-1 and PD-L1 are types of proteins found on cells in your body. PD‑1 protein is found on immune cells called T cells. It normally acts as a type of “off switch” that helps keep the T cells from attacking other cells in the body. PD-1 attaches to PD‑L1, a protein found on some normal (and cancer) cells. This interaction basically tells the T cell to leave the other cell alone and not attack it. Some cancer cells have large amounts of PD‑L1, which helps them hide from immune attack.
Therapies that target either PD-1 or PD-L1 can stop them from attaching and help keep cancer cells from hiding.
Learn more about KEYTRUDA, a type of immunotherapy that works by blocking the PD‑1 pathway.
KEYTRUDA can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. These problems may happen anytime during treatment or even after your treatment has ended.
Information Source: https://www.keytruda.com/how-does-keytruda-work/
Immunohistochemical
Which test is best for MSI and PD-L1 testing
IHC – Immunohistochemical or “Molecular Profiling”
Both work about the same in terms of results but –
- IHC: Fast 3-5 day turnaround versus Molecular Profiling (4-6 weeks) This allows for quicker treatment response.
- IHC and Molecular Profiling results agree 92% of the time
- IHC is inexpensive at approx $500.00 versus Molecular Profiling – $5,000 to $10,000
Clinical Trial Websites
What are MSi-high /dMMR Cancers
In normal cells, a system called DNA mismatch repair (MMR) corrects errors that occur during DNA replication. Defects in MMR can lead to microsatellite instability-high (MSI‑H), which can be found in many types of cancer. MSI‑H or mismatch repair deficient (dMMR) tumors have accumulation of errors in genetic sequences that are normally repeated (called microsatellites)
HOW A TEST FOR MSI‑H/dMMR WORKS
Important View Immuno 101
Everyone’s cancer is different. To help develop a treatment plan that’s right for you, your doctor may order laboratory tests. These tests can evaluate your tumor for different biomarkers, including MSI‑H or dMMR. Some biomarkers are used to help select patients that may benefit from certain treatments, such as KEYTRUDA. Talk to your doctor to see if a laboratory test for the MSI‑H or dMMR biomarker is right for you.
- A tissue sample (biopsy) of your tumor is taken, and your doctor orders the test.
- Your doctor typically gets the results in 10 to 14 days.
- You talk with your doctor to discuss treatment options based on your results.
- You may begin treatment with KEYTRUDA if you and your doctor have decided it’s right for you.